“When you cut your finger on a table saw, you don’t call up Kaiser and say, ‘Ok, where am I supposed to go? Am I supposed to go to the hospital that’s 15 minutes away? Am I supposed to go to the one that’s 30 minutes away?’”
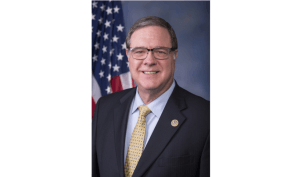
Rep. Ed Orcutt used a personal story to demonstrate one of the basic principles behind a bill up for debate on Monday. Orcutt said he cut his finger on a table saw in November, and has been surprised by two medical bills that have arrived since, months apart.
The House bill, which passed off the House floor in a bipartisan 84-13 vote, is meant to combat the practice of balance billing.

The Morning Wire: Keeping you informed on politics, policies, and personalities of Washington State.
Balance billing, also called “surprise billing,” is when a patient’s billed by an out-of-network provider for the difference between what their insurer reimbursed and what the provider charges.
As Orcutt referenced above, surprise billing happens in some cases when a person goes to an out-of-network hospital for emergency care — in his case, when he cut his finger on a table saw. Another common example is when a patient goes to an in-network facility, but is treated by an out-of-network provider who works there.
The bill that passed off the House floor today came at the request of the Insurance Commissioner (OIC). The OIC found that patients who are balance billed pay four to five times the amount they would’ve paid for the same services in-network, on average.
Under the bill, balance billing is prohibited for emergency services and for non-emergency surgical and related services (like labs and anesthesiology) provided at in-network hospitals and surgical centers.
A patient that receives those services pays the in-network amount specified in their plan, and the out-of-network provider can charge their insurance carrier a “commercially reasonable amount” for the service.
If carriers and providers can’t ultimately agree on an amount, the bill directs them to enter arbitration — a process that doesn’t include or concern the patient.
An exception to the balance-billing prohibition applies if an enrollee knowingly chooses an out-of-network surgeon over an in-network surgeon at least 72 hours before surgery at an in-network facility. In that case, the patient pays whatever their health plan requires to reimburse the out-of-network surgeon.
The bill also includes some transparency provisions, like a requirement that providers list the carriers with which they contract online.
State-regulated health carriers and insurers of public employees are subject to the bill. Medicaid isn’t, and self-funded group health plans can opt in.
The two representatives who argued against the bill, Reps. Joe Schmick and Drew Stokesbary, said that they support the ideas behind the bill. Schmick said that he was looking forward to voting for the bill, eventually.
“I’m just not quite there yet,” Schmick said. “This bill has come a long ways, where stakeholders have been involved. And now we’re just down to tweaking. And I know that nobody likes to have a balance bill come to their home. And I think we are going to get it accomplished.”
Stokesbary said that he was concerned the bill would take away existing incentives for carriers and providers to negotiate for lower prices.
“If we do this wrong, we’re going to remove that incentive for the providers to ever negotiate better deals, and we’re going to raise the cost of health care for everyone,” Stokesbary said. “And I know that’s not what any of us want to do.”
Orcutt pushed back on that argument, saying the current system doesn’t necessarily lead to negotiations that work out well for the patient.
“If a hospital or some other provider can just walk away from the negotiation with the insurance company and say, ‘Whatever, pay me what you’re going to [and] I’ll just get it from the patient later,’” Orcutt said, “that takes away the incentive to sit down and negotiate and get to lower health care prices.”
Now, the bill heads to the Senate. A bill aimed at balance billing passed out of the House in 2017 and 2018, but stalled in the Senate. Rep. Eileen Cody was the lead sponsor on the last bill, and is the lead sponsor on this year’s bill as well.
“Imagine having to go to the hospital and having surgery,” Rep. Cody said. “Everything goes well, you go home, and several months later you get a surprise bill from an anesthesiologist. You expected in-network status but one of the health care providers was out-of-network and you’re in the middle of a billing dispute. That’s wrong and I’m proud the House has once again passed legislation to end this practice.”
This story was cross-posted on our sister site, State of Reform.
Your support matters.
Public service journalism is important today as ever. If you get something from our coverage, please consider making a donation to support our work. Thanks for reading our stuff.